What Other States Could Learn from Maryland’s Model to Curb Healthcare Costs
Mike Stitcher and Kristen Geissler
Maryland transformed its hospital payment system in 2014 and has curbed cost growth and improved patient outcomes. With Washington encouraging state-level innovation, what can other states learn from Maryland’s success?
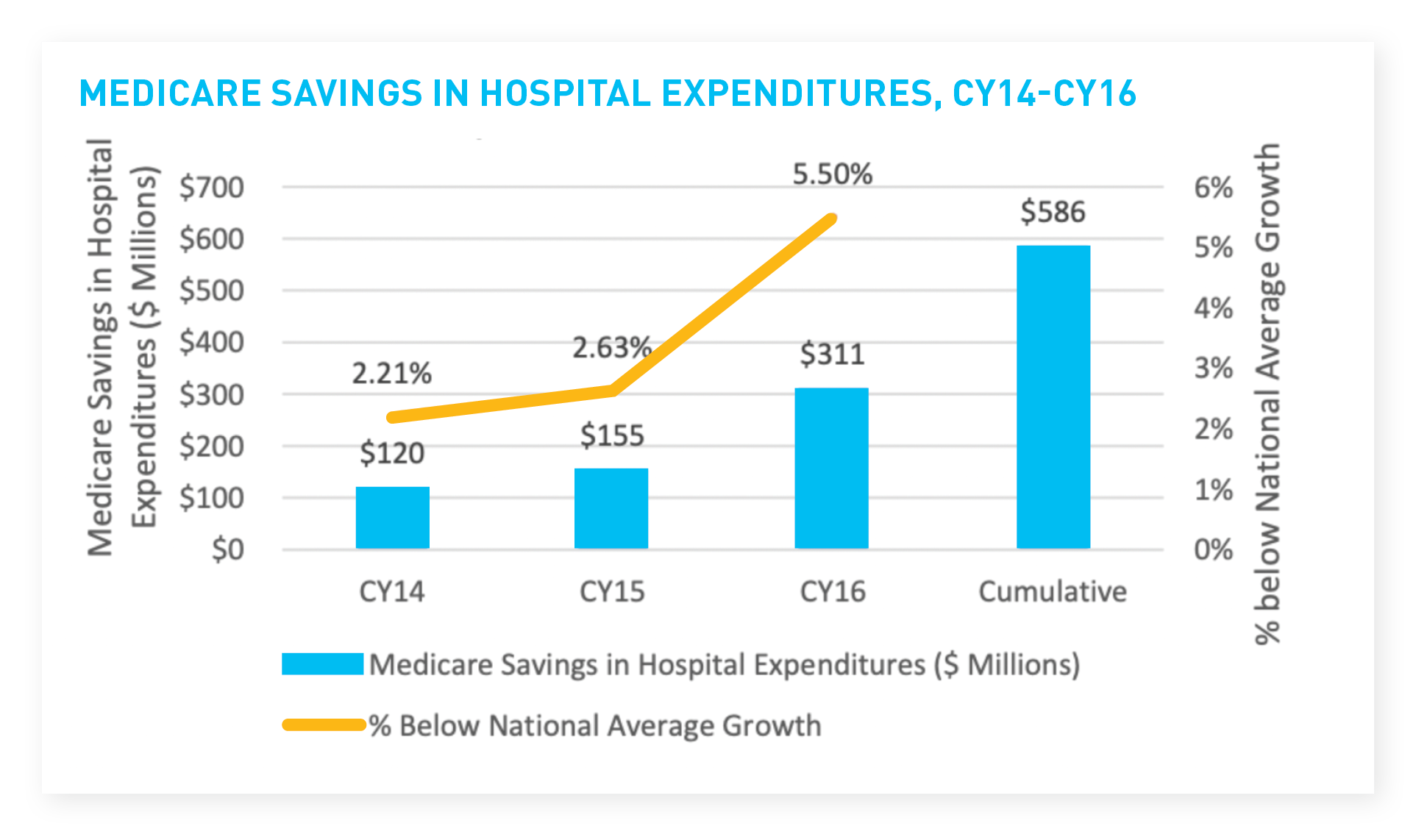
Starting about five years ago, the leaders of Maryland’s healthcare system undertook a transformation in the way the state manages costs and reimburses providers. The reforms not only generated more than $500 million in Medicare savings, but also managed to drive down costs while improving patient outcomes—meaning fewer hospital readmissions, trips to the emergency room and complications from medical procedures. While Maryland’s healthcare system is unique in the US, the story of how state officials reduced costs by improving care offers powerful lessons for the policymakers, regulators and industry leaders seeking solutions to challenges plaguing American healthcare.
For a brief explanation of how Maryland’s system works, see the sidebar below.
Since the 1970s, Maryland has had a sweet deal with healthcare regulators in Washington, DC: Keep the state’s inpatient cost growth below national trends, and the federal government will subsidize payments for Medicare and Medicaid services in the state, waiving a common payment rule.
But after the passage of the Affordable Care Act in 2010 and a push by Medicare to save more money, nothing was certain. And despite regulated rates for services, Maryland’s costs were accelerating faster than national averages.
That’s what Maryland healthcare officials were facing as the calendar turned to 2012. Maryland’s Health Services Cost Review Commission (HSCRC), which regulates the state’s all-payer healthcare system, ran the numbers on when costs would rise above the national average, putting the Medicare waiver in jeopardy. The answer: in about three months.
“So we took some emergency action to buy time,” said Patrick Redmon, then the executive director of the HSCRC and now a director in BRG’s Baltimore office.
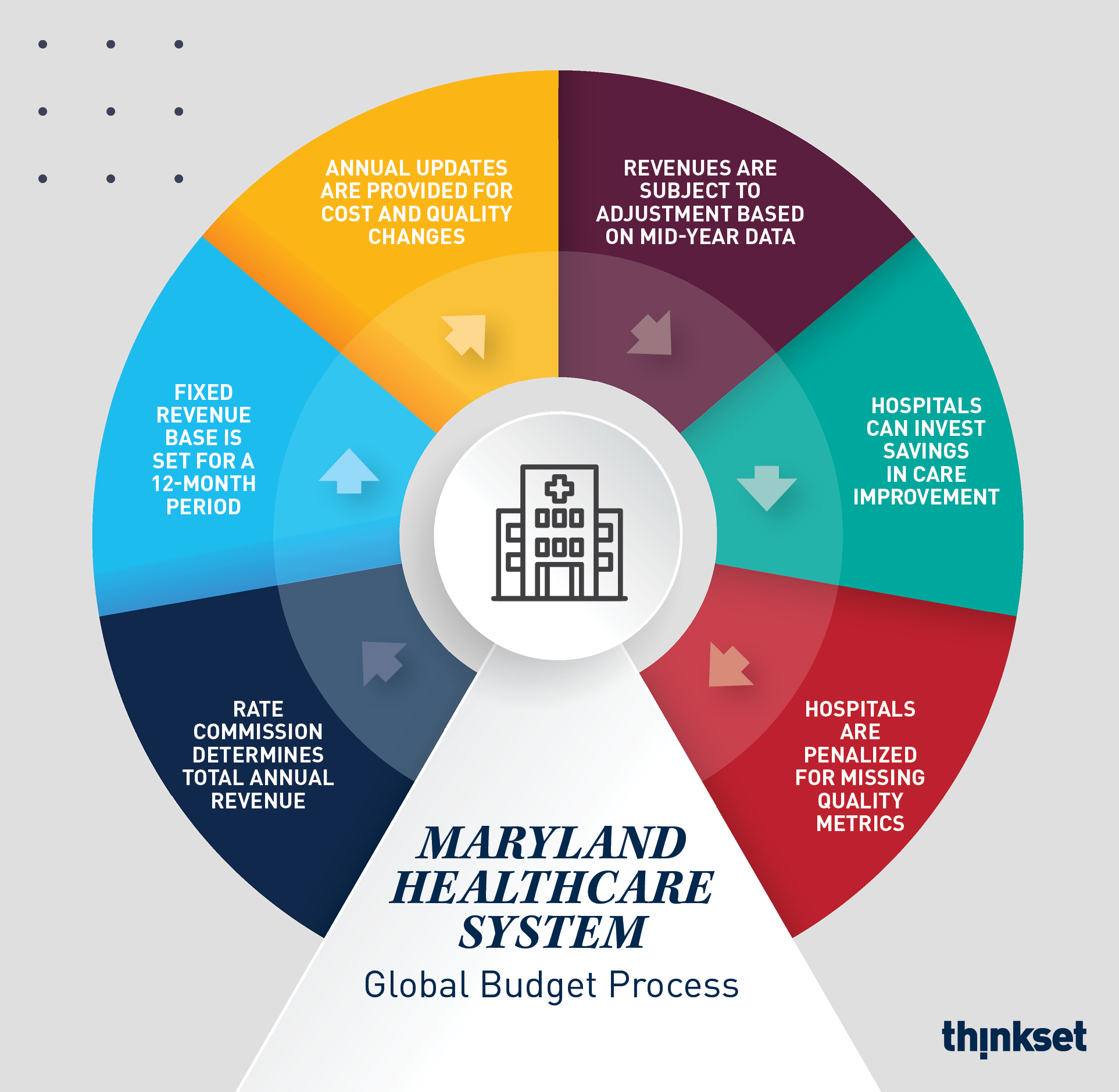
The HSCRC commenced negotiations with the Centers for Medicare and Medicaid Services (CMS) to revise the Medicare waiver and create a new hospital payment model, which shifted from a regulated fee-for-service model to all-payer global budgets. That meant that hospitals would be given an annual budget based on their patient population and could reinvest the difference if they spent less than anticipated.
This crucial change flipped the economic incentives for providers. Hospital executives who had previously seen robust patient demand as necessary to remaining solvent now had an incentive to keep patients out of the hospital. Taking care to ensure the regulatory changes didn’t harm patients, Maryland and CMS officials also added financial penalties for hospitals that failed to meet key quality standards.
The five-year demonstration contract Maryland negotiated with CMS, which took effect in 2014, required Maryland to limit per-capita patient cost growth to 3.58 percent, generate $330 million in savings to Medicare over the course of the contract, reduce its 30-day readmission rate to the national average and hit other quality and cost outcomes.
It was a tall order, to say the least.
Source: Maryland Department of Health, Maryland’s All-Payer Hospital Model Results Performance Year Three, HSCRC (March 2018), available at: https://hscrc.maryland.gov/Documents/Modernization/Maryland%20APM%20Performance%20Report%20-CY2016_3_9_18.pdf
A remarkable transformation
What happened over the next few years was nothing short of remarkable. The new incentives forced executives and practitioners to rethink the amounts and types of care they recommended. The incentives led doctors to pay closer attention to patients as they left the premises, in order to make sure they didn’t have to come back. And the incentives made Maryland’s healthcare system more effective at putting patients in the right level of care: sending them to ambulatory care rather than emergency rooms, for example, or establishing home care rather than sending elderly patients to nursing homes.
In 2018, the HSCRC wrote that it was on track to meet its obligations and deliver “hospital Medicare savings of $586 million and total hospital and non-hospital Medicare savings of $461 million through the end of calendar year 2016.” The commission also noted that it had improved quality and reduced complications for patients.
CMS was so satisfied with the results that it renewed and expanded Maryland’s Medicare waiver in January 2019. The new “Total Cost of Care Model,” to be piloted over the next five years, puts Maryland on a path to further bend the cost curve by expanding the performance metrics beyond the hospital system and into other care settings.
Just as impressive as the care coordination was the political unity around Maryland’s reforms. It was a bipartisan effort at both the state and national levels—a system set up under President Obama and sustained under President Trump.
What can America learn from the Maryland model?
Maryland is the only state still operating with a Medicare waiver dating back to the 1970s. That’s simply not an arrangement that CMS will entertain for other states—at least for now. Without that incentive, other states would be hard-pressed to summon the political will to create similar regulatory structures.
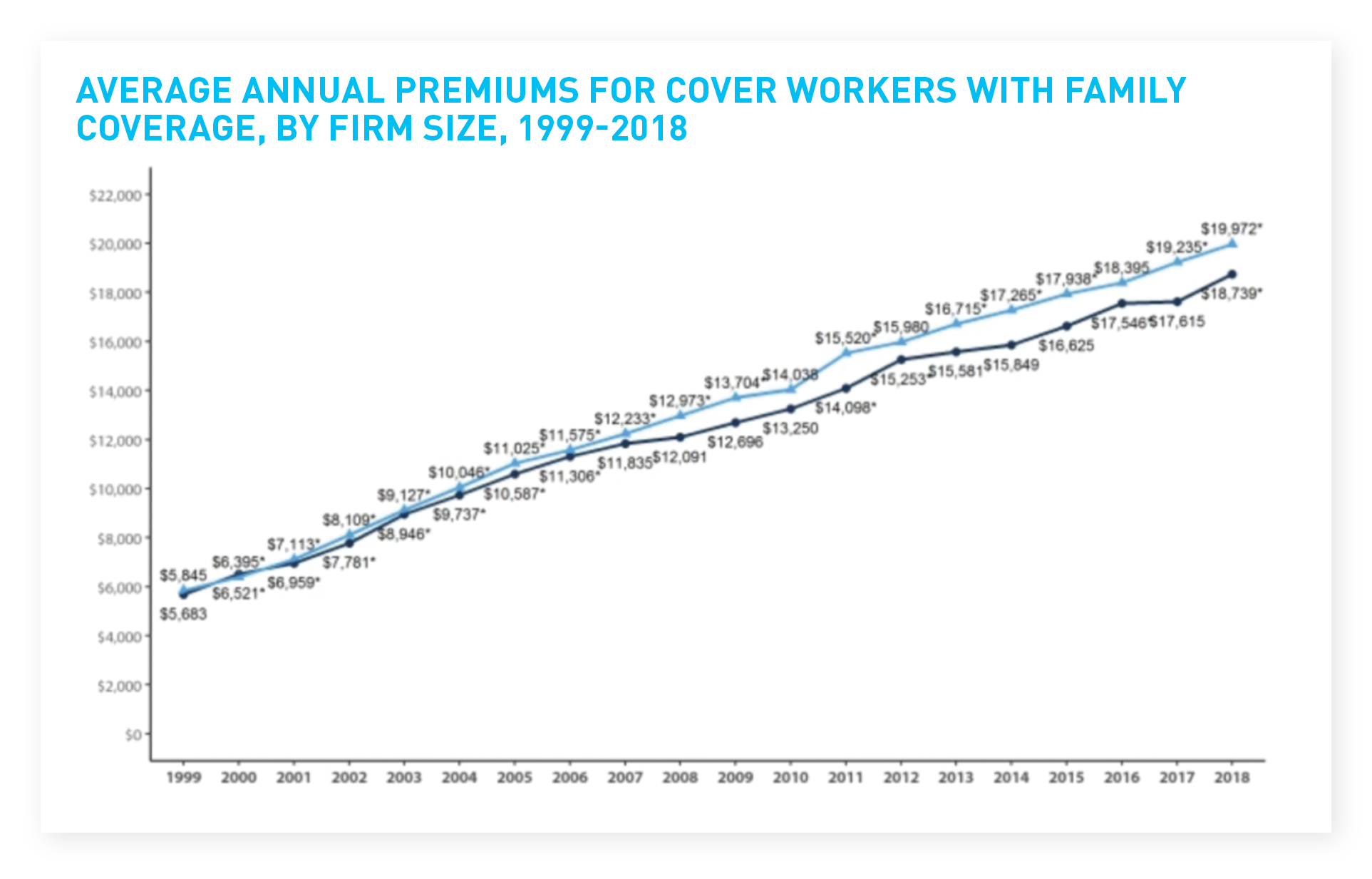
However, everyone from consumers to employers and policymakers is desperate for innovative solutions to curb cost growth. The average family paid a $19,616 premium for health insurance in 2018, up 20 percent from 2013 and 55 percent since 2008. The collective concern is such that viable contenders for the presidency have announced plans to overhaul the healthcare system entirely.
Source: Kaiser Family Foundation, 2018 Employer Health Benefits Survey (October 3, 2018), available at: https://www.kff.org/report-section/2018-employer-health-benefits-survey-section-1-cost-of-health-insurance/
In that context, global patient-based budgets—like those piloted in Maryland, but without the regulatory component—have attracted a great deal of interest lately. Maryland’s success with those budgets contains powerful lessons for leaders at the state and federal levels, and for executives at providers and payers.
We’re starting to see encouraging experiments. Pennsylvania, with the blessing of CMS, has embarked on a trailblazing initiative with five economically challenged rural hospitals. Because the state’s regulators don’t set all payers’ rates, the Pennsylvania model assigns a proportion of global budgets to the five participating payers.
Although the Pennsylvania Rural Health Model is in its infancy—legislation creating it passed early this year—the state’s Department of Health says over a dozen other states have been in touch to learn more about the program. CMS has also indicated an interest in using lessons learned from Maryland and Pennsylvania, and from an accountable care organization model being piloted in Vermont, to try out similar programs in other states.
How global budgets align incentives—and political forces
While much of the political conversation around healthcare today is about profits, the problem for most providers is simply staying out of the red. Executives at rural and safety-net hospitals across the country are battling demographic and socioeconomic forces far more powerful than any operational changes they can make.
Efforts are underway to expand all-payer global budgets in rural areas. But what can work in urban areas? Or in regions with mixed population density? And can some version of the Maryland model work without a Medicare waiver that originated during the Nixon administration?
That’s the question many states and healthcare organizations are asking. The Commonwealth Fund, a nonprofit working on healthcare accessibility, wondered if an all-payer global budget could work in the Bronx, with a population of 1.46 million and a poverty rate of 31.5 percent.
“Bringing all the hospitals together under global budgeting,” the authors wrote, “could allow for the design of a transformed health system with alignment for the health of the population and with the engagement of community leaders and public health agencies.”
The great unifier in Maryland has been a shared desire to keep the Medicare waiver. But the state’s unique conditions have made it a petri dish for healthcare reform, and other regions and states can extract actionable lessons from the first five years of Maryland’s all-payer experiment. Having worked on the Maryland model, and then with other states seeking similar outcomes, the authors have learned a few of overarching lessons, including:
Carrots and sticks: Players in Maryland’s hospital system understand the outcomes they need to achieve and the consequences if they fall short. Hospitals that fail to control costs or let quality slip risk losing substantial revenue. If Maryland’s system as a whole fails to deliver on cost and quality of care, it would lead to a more expensive system for all involved. Whatever the local rules and regulations, hospitals and payers need to see the financial benefit of participation; they face severe consequences if quality of care declines.
Hospitals can have it all: Given correctly aligned incentives and guardrails, hospitals can innovate to drive costs down and improve care. Global budget models do not mean rationed care, as long as they are coupled with quality oversight and flexible budgeting. Whether hospitals are monitored under a state regulatory board (Maryland) or public–private oversight body (Pennsylvania), the pressure on costs and quality must be equal, with tools to make quick changes based on unforeseen events.
Shared vision = broad support: The public is desperate for change that will reverse healthcare cost trends, as evidenced by broad public support for Medicare for All and resistance to any rollback of the Affordable Care Act that could make matters worse. That gives policymakers significant leeway to move forward with bold solutions—such as changing the type of care people receive or the services offered at their local hospitals— that could drastically change the status quo.
It's time for bold visions in healthcare
Policymakers at the local and state levels should not be cowed by gridlock over healthcare at the national level. Local leaders who put forward sensible and strategically sound proposals for healthcare reform that feature realistic cost controls will find a receptive audience in the public, not to mention the payers and providers dealing with that anger on the ground.
As experiments in Maryland, Vermont and Pennsylvania move forward, other states will have more data to build on what is working and adjust on lagging aspects. And as anyone working in healthcare payment reform knows, CMS giving a tacit greenlight for local innovation puts wind in reformers’ sails.
Some aspects of the Maryland model may not work in other states, but its success should give hope to policymakers and executives during a frustrating time in American healthcare. When the incentives of the public and private sectors, and of patients and payers, are aligned, it’s possible to bend the cost curve, improve patient outcomes and set the course for further innovation.
The Maryland Model: How—and Why—It Works
In other states, Medicare pays about 85 cents for each dollar of hospital costs, and private insurers cover the rest. The gap amounts to tens of billions of dollars a year on a national level.
But Maryland has long used a regulatory rate-setting process (not just the state-run Medicaid program) to create statewide reimbursement rates for all payers; in most states, each private payer negotiates its own rates with providers.
Maryland’s universal rate-setting gives state regulators the power to impose cost controls on providers; that’s what convinced federal officials to cover 100 percent of Medicare costs, so long as the state met its cost-containment goals.
For decades, Maryland’s system worked like the rest of US healthcare: providers got paid for each service, so the more patients they saw, the more procedures they performed, and the more time people spent in hospitals, the more revenue providers raked in.
But five years ago, state officials conceived of and implemented a new universal-budgeting model, which sets an annual budget for each provider based on the patient population they serve. Providers that can hold costs below their annual budgets keep the difference—a crucial source of potential capital for struggling hospitals.
The universal budget also includes penalties for failing to meet quality of care measures like hospital readmissions, ensuring that providers can’t manage budgets by cutting corners on treatment.